A Word About Inflammation
It is important to understand that regenerative medicine is based on a cellular process of repair. After tissue damage has occurred, such as a tendon or ligament tear or a bone fracture, the body increases blood flow to the area and sends out signals to its repair system to recruit and deliver the proper cells and proteins to the damaged area needed for healing. Therefore, the goal of regenerative medicine is to augment this process. If a condition is chronic in nature, the injury site may be stagnant and needs to be converted back to more of an acute healing mode, so the body can properly recruit the proper cells for repair. Perhaps the best way to think about this organic process is to compare it to another, more familiar one. In order for a plant to produce flowers, it needs to have a stable home in nutrient rich soil and have lots of water and sun. If a plant is struggling to produce flowers, this could indicate a situation where plant has been physically damaged or it is not in a conducive and nurturing environment. Before you dig up the plant and put a new one, one should consider what is causing the problem in the first place as planting a new plant in nutrient poor soil will likely lead to the same result, which is similar to chronic inflammation where the body is just not capable of turning the situation around. A regenerative approach would call for aerating the soil around the ailing plant to convert it to more an acute process, adding nutrients to the soil with the addition of fertilizer and perhaps Scott’s Miracle Grow (which can be compared to using nutrient rich placental/amniotic tissue) to enhance the environment and convert it back to a state that is optimal for the plant to thrive and eventually produce flowers. In the body, this technique is what we are trying to simulate by agitating a chronically damaged site to convert it to an active repair site and them stimulating new tissue growth by seeding the area with stem-cell based technologies which rejuvenate the “soil” via the deliverance of growth factors and extracellular matrixes (proteins) that the body can utilize to heal itself.
So, What's the Deal with Cortisone?
Cortisone is one of the main hormones that are naturally released by our bodies as a result of stress or injury. Cortisone injections contain a synthetic version of this hormone and are traditionally injected directly into the injured area to reduce the inflammation that occurs with tissue damage, therefore reducing pain. While it is a strong anti-inflammatory, cortisone works in a totally different way than the regenerative medicine approach and can often be associated with some very serious downsides. Unfortunately, cortisone is often mistaken to be a miracle drug due to its ability to almost instantly get rid of pain. In reality, it actually retards the body’s natural response to injury and ultimately blocks the repair process. Less pain? Yes, however cortisone almost instantly reduces or eliminates the proper inflammatory response associated with either tendon and muscle injuries. Furthermore, it has been well documented in the literature that cortisone use near tendons can compromise the tendon to the point where it can eventually fail and rupture. Cortisone by an acute bone fracture will prevent it from healing. Repetitive cortisone injections into an arthritic joint will actually cause further cartilage degradation and actually lead to an advancement of the arthritis. So is it all bad?
While we usually try to avoid cortisone injections when we can, one or two at the most may calm severe/chronic swelling and pain. In very limited cases, it helps break the inflammation cycle of conditions such as capsulitis, morton’s neuroma or plantar fasciitis. It can bring almost immediate short-term relief from pain and, sometimes, longer-term relief which can help a patient get through more meaningful therapeutic exercises necessary to address the underlying condition.
It’s very important to note that we never inject cortisone into the Achilles tendon. Cortisone can make the Achilles injury worse and increase the risk of a complete tendon rupture.
Cortisone injections do not stimulate healing, nor do they address the core issue of the pain, whatever that may be. The benefit of regenerative medicine is that unlike cortisone injections, use of stem cell-like therapies to stimulate healing have never been associated with a derogatory effect nor do they lead to weakened or damaged tissues. Rather, they regenerate the body’s ability to heal itself.
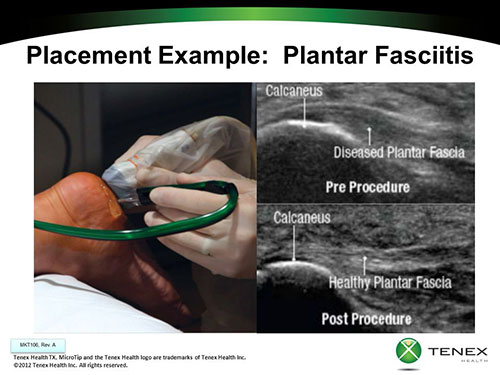
Converting Chronic to Acute

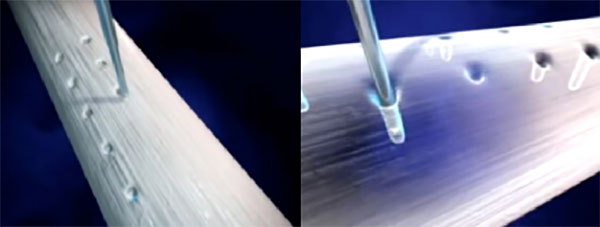
In a situation where inflammation has been present for an extended period of time, the body has likely given up on the healing process. In order to get the area ready for productive healing through tissue regeneration, it must be converted back to an acute process so that the body can send out signals to its repair cells and attract them to the damaged tissue. This can be done in a number of ways. Traditional open surgical repair is one way to “stir the pot”. In the event a ligament or tendon is repaired via a traditional open surgical approach, use of an amniotic tissue matrix membrane or injection into/around the repair site will insure that there are additional nutrients (growth factors and proteins) are available to further stimulate an optimal healing environment. In the event a more minimally invasive method is chosen, the amniotic derived tissue may be injected into the repair site. To optimize healing, the site may benefit from a procedure that is geared towards micro-debriding the soft tissue and therefore causing a controlled amount of acute damage to encourage the body to convert the site into the more productive form of inflammation that can trigger the natural repair process.