 Rearfoot fractures of either the heel bone (calcaneus) typically occur after a high impact/velocity injury, such as a fall from height or motor vehicle accident. Due to the force of the injury, the damage is often extensive and often requires surgery. These injuries are also closely associated with the development of post-traumatic arthritis of the subtalar joint (rearfoot).
Rearfoot fractures of either the heel bone (calcaneus) typically occur after a high impact/velocity injury, such as a fall from height or motor vehicle accident. Due to the force of the injury, the damage is often extensive and often requires surgery. These injuries are also closely associated with the development of post-traumatic arthritis of the subtalar joint (rearfoot).
Causes of a Calcaneal Fracture
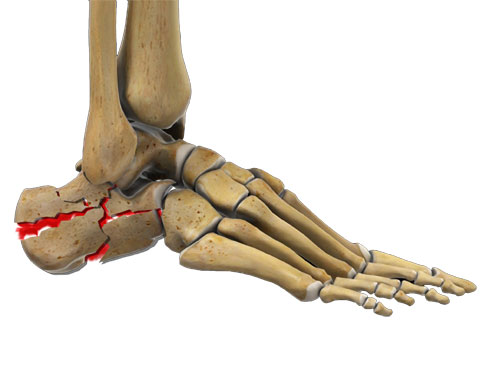
A calcaneal fracture occurs when an excessive force crushes the heel bone against the talus (the lowest bone of the ankle). The joint between the calcaneus and the talus is known as the subtalar joint, and it is an essential biomechanical component of flexing, standing, and walking and couples with the ankle joint for dynamic motion. This joint is often involved in these types of facture which can lead to long term problems with the joint such as chronic pain, stiffness and the development of arthritis.
 Treating a calcaneal fracture can be extremely tricky, because the fracture is rarely a clean break like you might see in a broken shin or arm. Think of the calcaneus as an egg… with in intact shell it is hard to break when you squeeze it in the palm of your hand, however, if there is any defect or crack in the surface, any abnormal pressure to the shell cause it to crumble as the center is soft and sponge-like. When the calcaneus fractures, the hard outer layer can break into multiple irregular fragments and fold in on itself, just like an egg with a broken shell.
Treating a calcaneal fracture can be extremely tricky, because the fracture is rarely a clean break like you might see in a broken shin or arm. Think of the calcaneus as an egg… with in intact shell it is hard to break when you squeeze it in the palm of your hand, however, if there is any defect or crack in the surface, any abnormal pressure to the shell cause it to crumble as the center is soft and sponge-like. When the calcaneus fractures, the hard outer layer can break into multiple irregular fragments and fold in on itself, just like an egg with a broken shell.
Types of Calcaneal Fractures
There are several types of fracture patterns that can occur with trauma to the heel bone. Some have more simple patterns that do not involve the joint and usually heal without any long term issues while others are more complex with fragment displacement and extend into one of multiple joints and are very challenging to get to heal properly, often requiring surgical intervention to optimize healing.
- Intra-articular fractures. These involve damage to the cartilage between the joints, and are considered the most serious type of heel fracture. These have a high correlation with the eventual development of post traumatic arthritis of the involved joint (s)
- Avulsion fractures. A fragment of bone is avulsed away from the calcaneus from the pulling from the Achilles tendon or another ligament.
- Multiple fracture fragments. This is also known as a crushed heel injury and is more common with higher impact injuries such as a fall from height or automotive accident.
- Stress fractures. While most calcaneal fractures are caused by a trauma, a calcaneal stress fracture can result from overuse or repetitive trauma (like high volume running or jumping).
Symptoms of a Calcaneal Fracture
- Sharp, severe pain
- Extensive swelling and bruising in the heel region
- Inability to bear weight
- A general pain in the heel that gradually worsens could be a sign of a stress fracture. This will typically on hurt during activity and gets better with rest.
Diagnosing Calcaneal Fractures
 If you have recently experienced a trauma and are experiencing symptoms of a calcaneal fracture, visit your foot and ankle specialist. You doctor will evaluate your foot for swelling and other signs of a fracture or joint damage. X-ray imaging can be helpful in making a diagnosis. Your doctor may also order a CT scan to get a better idea of the pattern of the fracture, to determine whether surgery is needed.
If you have recently experienced a trauma and are experiencing symptoms of a calcaneal fracture, visit your foot and ankle specialist. You doctor will evaluate your foot for swelling and other signs of a fracture or joint damage. X-ray imaging can be helpful in making a diagnosis. Your doctor may also order a CT scan to get a better idea of the pattern of the fracture, to determine whether surgery is needed.
Depending on the cause of your injury, your foot and ankle specialist may also examine you for an ankle or mid-foot injury, or refer you to another specialist to check for injuries beyond the foot. About 10% of patients with calcaneal fractures also suffer a back injury called a Lumbar spinal burst fracture. This occurs when a vertebra in the lower-mid back is crushed. Please let you doctor know if you are also experiencing any back pain.
Calcaneal Fracture Treatment
Heel bone fractures are notoriously difficult to treat, and usually require prolonged healing times. Your foot and ankle specialist will assess your injury and determine whether to treat the fracture surgically or non-surgically.
Conservative Treatment
Conservative treatment is most appropriate for simple, non-displaced fracture patterns, especially if they do not involve the joint. A conservative, non-invasive treatment regimen may also be recommended for patients who are not good candidates for surgery. Smokers, elderly patients, and patients with diabetes or vascular disease may be at higher risk for surgical complication, such as an infection or blood loss.
As severe as calcaneal fractures can be, studies have shown that non-surgical treatment can be very nearly as effective as surgical treatment in the right individuals. Typically, non-surgical treatment involves:
- Non-weight bearing status for up to 10-12 weeks
- Immobilization in a cast, fracture boot or splint for 8-10 weeks
- Elevation of the foot. When resting, prop your foot up on stools or pillows to keep it above your heart.
- Icing. Apply malleable freezer gel packs to the anterior ankle. Change every 2-3 hours to help with swelling
- Compression. Wrap your heel in a compression sock or ace bandage.
- Pain medication. Your doctor may prescribe you pain medication or you can take over-the-counter NSAIDs, such as Ibuprofen and Naproxen. Please note that narcotics in our practice are extremely restricted and are NOT a good long term solution.
- Physical therapy exercises. After 2 weeks, practice drawing a figure-8 with the toes to increase your range of motion in the ankle.
Surgical Treatment
- Open Surgical Approach: Surgical correction of a calcaneal fracture takes an extremely skilled surgeon, and is inherently risky. Your surgeon will reconstruct the heel bone to something close to its original shape. Because each fracture is different, each surgical procedure is highly individualized.
Typically, surgery cannot begin until the swelling has gone down, about 10-14 days following the trauma. Operating on an excessively swollen foot may lead to healing problems and it can increase the risk for infection.
The surgery is generally performed through an open incision on the outer side of the heel. The surgeon then carefully repositions the fragments and fixes them into place with anatomically designed screws and plates.
- Percutaneous Approach: This is a minimally-invasive surgical technique that can be performed on some less complex fractures (less than 10%). The surgeon makes a small incision and pierces the pieces of fractured bone with surgical wire. The surgeon can then manipulate the pieces into place. Once the fragment position is optimized, then a plate can be slid under the skin and fixated to the bone with a few screws placed through minute incisions along the periphery of the plate or with multiple screws placed strategically around the fracture without a plate.
Complications of Calcaneal Fracture Surgery
Surgical correction of a fractured heel bone is a risky procedure. Common complications may include:
- Infection. Unfortunately, these can occur. In mild cases, this may be treated with oral antibiotics. In more severe cases, the entire surgical may become compromised and require a removal of hardware and any infected tissue or bone. Osteomylelitis is a severe deep-wound infection that affects the bone, and the calcaneus is particularly vulnerable following this type of injury. If this occurs, this may require multiple surgeries in order to resolve the infection, long term use of IV antibiotics, and in some extreme cases can lead to limb loss if the infection becomes a threat to your health.
- Would healing problems. Because circulation to the heel’s soft tissues is relatively weak, the surgical site may not heal properly and may require additional wound care and/or skin grafting.
- Subtalar arthritis. This is a chronic pain condition which commonly affects patients with healed calcaneal fractures. If this occurs, at some point you may need to undergo an additional procedure to fuse the affected joints which most commonly the subtalar joint.
- Nerve damage. You may experience permanent numbness at the surgical site. In some cases, the sural nerve (which runs through in incision site) may become entrapped in scar tissue and can become quite painful.
- Non-union: Sometimes the bone simply doesn’t heel. If this is the case, the use of a bone growth stimulator (non-invasive) may be beneficial. In more severe cases, this may require additional surgery to help the bone resume normal healing.
 Recovery from Calcaneal Fracture Surgery
Recovery from Calcaneal Fracture Surgery
Following surgery, your foot and ankle specialist will likely immobilize your foot in a splint to allow the bone and joints time to heal. You should follow the at-home treatments recommended for non-surgical patients, including rest, ice, elevation, and compression.
You should avoid bearing weight on the foot for 10-12 weeks until it is sufficiently healed. This is often determined by serial x-rays performed in the office during your follow-up visits. Once you are allowed to bear weight on the foot, Dr. Perler usually sends you for physical therapy who will help you get back to full weight bearing and out of the boot over the following month. Also, many patients will benefit from either custom or over the counter arch supports.
 Dr. Perler has a special interest in treating and rehabilitating ankle sprains and chronic ankle instability. He will evaluate the ankle during your initial visit, looking for stability and any evidence of abnormal ankle rotation. This helps identify if any ligaments are injured and to what extent. Muscle testing is also performed to assess weakness or injury.
Dr. Perler has a special interest in treating and rehabilitating ankle sprains and chronic ankle instability. He will evaluate the ankle during your initial visit, looking for stability and any evidence of abnormal ankle rotation. This helps identify if any ligaments are injured and to what extent. Muscle testing is also performed to assess weakness or injury.
 Soft tissue injuries to the foot and ankle can be mild and have a relatively rapid and straightforward recovery while other more severe soft tissue injuries can lead to lingering long-term issues such as chronic ankle weakness, instability, pain, swelling and eventually to degradation of the joint. Inversion ankle injuries (ankle sprains) are perhaps the most common presenting injury at your local ER or urgent care facilities, yet many times if no fractures are seen on x-ray, the patient is told the “good news” that it is just a sprain or strain and sent home with some basic information on sprains. However, this can be misleading as ligament tears, cracked cartilage, and tendon ruptures cannot be diagnosed on x-rays alone.
Soft tissue injuries to the foot and ankle can be mild and have a relatively rapid and straightforward recovery while other more severe soft tissue injuries can lead to lingering long-term issues such as chronic ankle weakness, instability, pain, swelling and eventually to degradation of the joint. Inversion ankle injuries (ankle sprains) are perhaps the most common presenting injury at your local ER or urgent care facilities, yet many times if no fractures are seen on x-ray, the patient is told the “good news” that it is just a sprain or strain and sent home with some basic information on sprains. However, this can be misleading as ligament tears, cracked cartilage, and tendon ruptures cannot be diagnosed on x-rays alone.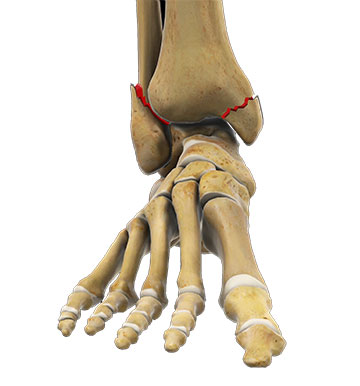 What Causes an Ankle Fracture?
What Causes an Ankle Fracture? Ankle Fracture Treatments
Ankle Fracture Treatments Ankle fractures often require surgery to replace the fractured pieces to normal anatomic alignment and put the ankle joint in the correct position. The surgical treatment is known as an open reduction and internal fixation or ORIF. This is usually accomplished with the help of specially designed plates and screws. There are several reasons why an ankle fracture will require surgery. If the fracture is displaced or angulated, and the ankle joint is no longer aligned, surgery is required to realign the ankle joint. It is essential to align the ankle fracture to within 2 millimeters of original position for optimal long-term results. Ankle fractures involving joint cartilage can lead to arthritis in the joint. It is especially important that ankle fractures are reduced to return the anatomy to its normal position and alignment.
Ankle fractures often require surgery to replace the fractured pieces to normal anatomic alignment and put the ankle joint in the correct position. The surgical treatment is known as an open reduction and internal fixation or ORIF. This is usually accomplished with the help of specially designed plates and screws. There are several reasons why an ankle fracture will require surgery. If the fracture is displaced or angulated, and the ankle joint is no longer aligned, surgery is required to realign the ankle joint. It is essential to align the ankle fracture to within 2 millimeters of original position for optimal long-term results. Ankle fractures involving joint cartilage can lead to arthritis in the joint. It is especially important that ankle fractures are reduced to return the anatomy to its normal position and alignment. 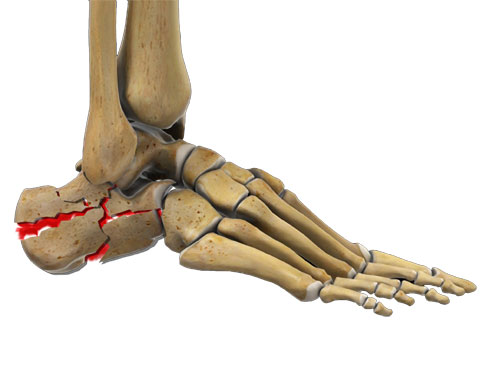 Rearfoot fractures of either the heel bone (calcaneus) typically occur after a high impact/velocity injury, such as a fall from height or motor vehicle accident. Due to the force of the injury, the damage is often extensive and often requires surgery. These injuries are also closely associated with the development of post-traumatic arthritis of the subtalar joint (rearfoot).
Rearfoot fractures of either the heel bone (calcaneus) typically occur after a high impact/velocity injury, such as a fall from height or motor vehicle accident. Due to the force of the injury, the damage is often extensive and often requires surgery. These injuries are also closely associated with the development of post-traumatic arthritis of the subtalar joint (rearfoot). Treating a calcaneal fracture can be extremely tricky, because the fracture is rarely a clean break like you might see in a broken shin or arm. Think of the calcaneus as an egg… with in intact shell it is hard to break when you squeeze it in the palm of your hand, however, if there is any defect or crack in the surface, any abnormal pressure to the shell cause it to crumble as the center is soft and sponge-like. When the calcaneus fractures, the hard outer layer can break into multiple irregular fragments and fold in on itself, just like an egg with a broken shell.
Treating a calcaneal fracture can be extremely tricky, because the fracture is rarely a clean break like you might see in a broken shin or arm. Think of the calcaneus as an egg… with in intact shell it is hard to break when you squeeze it in the palm of your hand, however, if there is any defect or crack in the surface, any abnormal pressure to the shell cause it to crumble as the center is soft and sponge-like. When the calcaneus fractures, the hard outer layer can break into multiple irregular fragments and fold in on itself, just like an egg with a broken shell. If you have recently experienced a trauma and are experiencing symptoms of a calcaneal fracture, visit your foot and ankle specialist. You doctor will evaluate your foot for swelling and other signs of a fracture or joint damage. X-ray imaging can be helpful in making a diagnosis. Your doctor may also order a CT scan to get a better idea of the pattern of the fracture, to determine whether surgery is needed.
If you have recently experienced a trauma and are experiencing symptoms of a calcaneal fracture, visit your foot and ankle specialist. You doctor will evaluate your foot for swelling and other signs of a fracture or joint damage. X-ray imaging can be helpful in making a diagnosis. Your doctor may also order a CT scan to get a better idea of the pattern of the fracture, to determine whether surgery is needed. Recovery from Calcaneal Fracture Surgery
Recovery from Calcaneal Fracture Surgery